Real stories
Delayed discharge from hospital: 'Hospital stays really affected mum'
Martin shares his mum's experience of delayed discharges from hospital and the impact it had on her.
I worked in social care for 40 years, including 16 years as director of social services in Liverpool, York and Barnsley, but it wasn’t until my mum, Sarah, was diagnosed with Alzheimer’s disease in 2018 that I really understood the gravity of what it is to live with it.
She’s in a care home now and getting very good care but for a while she was in sheltered accommodation where she wasn’t getting the support she needed. One big issue was dehydration – a common problem for people living with dementia – which led to repeated urinary tract infections (UTIs) and falls.
Getting admitted to hospital
As a result, she was admitted to hospital several times, which was incredibly frustrating given it could have all been prevented by helping her to stay hydrated.
The figures released by Alzheimer’s Society really ring true for me.
Every time mum went into hospital, she was kept in significantly longer than necessary. This was despite the fact she was well enough to leave and there was a care package in place for her to return home.
One bewildering example was the month she spent on a surgical ward. She had not had, and nor did she need, surgery – it was just the only place to put her. It was a busy, chaotic ward, not set up to meet the needs of someone with dementia.
I was away at the time. My professional background means I understand the system and how to navigate it, which can help me get mum the care she needs. Without me there, my sisters struggled to get answers. They struggled to get a meaningful response when they asked questions about why she was there and when she would be discharged.
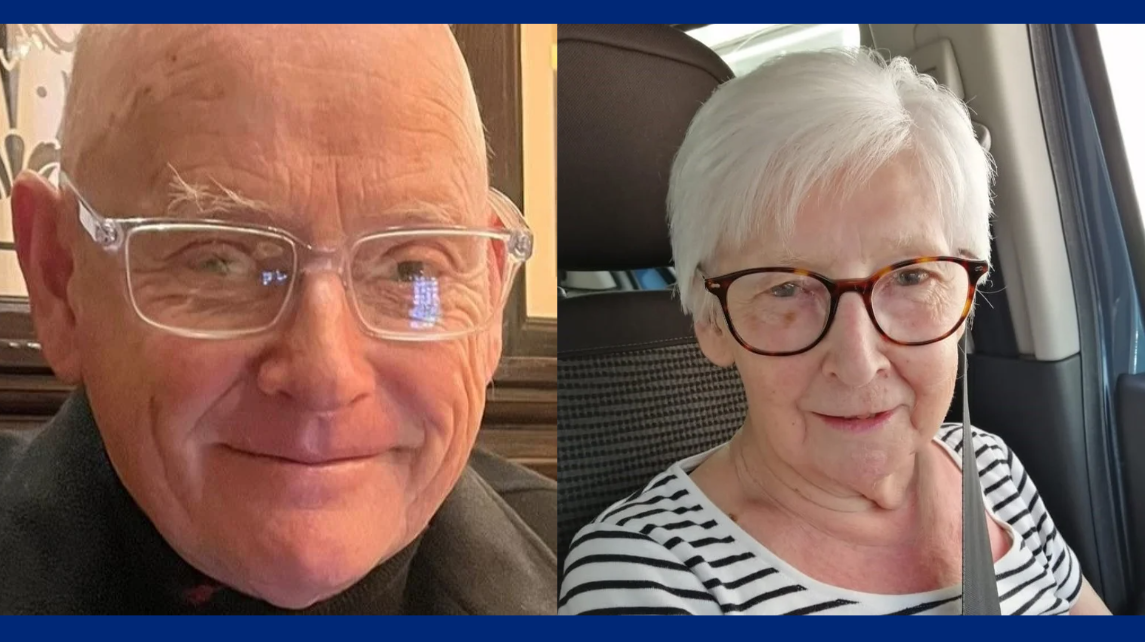
Martin and his mum, Sarah
When I got back, I ended up insisting that I was taking her home. Even then I had to argue with the staff over the medication she required. They wanted to keep her in several more hours to wait for it and took some persuading that I could pop back and collect it once I had settled her in back at home.
The result of multiple hospital stays
Those hospital stays really affected mum. I am generally very positive about the NHS and the staff who have looked after mum at various times have been very kind, but the system just isn’t set up to deal with dementia.
The staff don’t usually have the time or the training to talk to patients with dementia, get to know them and help them understand what’s happening.
As a result, she was confused and very isolated, which wasn’t good for her mental health. Her physical health has taken a hit too. If you don’t support someone with dementia to stay active, their mobility can decline very quickly.
Now she is in a care home, she’s getting much better support. They are better equipped to manage dementia, which prevents the need for disruptive hospital visits. With mum, for example, they are good at helping her stay hydrated, which in turn reduces the risk of UTIs and falls.
She’s finally getting the dementia-specific care she needs and the impact is really clear. Her physical health is good, she sleeps really well and she has people around her for company, which makes a huge difference to her mental wellbeing.
What needs to change
I don't subscribe to the view that the NHS is broken but at present it’s not geared up to provide for the longer-term care needs associated with dementia.
Preventing avoidable hospital admissions in the first place is crucial, improving dementia training and increasing support so people get the care they need at home.
There are solutions and improvements needed throughout the system and I have had the privilege of working on pilots in the North West that have proven to be better for both local services and the people they support.
I am pleased that the government is working on a ten-year plan for dementia health and social care – but I hope it makes the most of this rare opportunity.
It needs to learn from people’s experiences, consider examples like the initiatives I have worked on and look at the system as a whole. This won’t just free up precious acute care capacity in the NHS, it will make a huge difference to people living with dementia.
Delayed discharge from hospital
Figures show the true extent of delays to discharge from hospital for people living with dementia.



Gemma Beer
saysSylvia Rankin
saysLynne Issitt
saysJoseph Louis Lionel Vaz
saysJoanne
saysJoanne
saysChristina Knight
saysNazanin
saysChristine Leake
saysSusan Wilkie
saysCollette Otoole
saysJohn Swait
saysEsme Hagard
saysMartin
sayscarolyn chilver
saysFiona Fulford
says