Newcastle University: The Pri-Dem project
Learn about the background of the Pri-Dem project, the team behind it, and its aim to develop and evaluate acceptable, feasible and sustainable models of care, which are centred on the person receiving the diagnosis.
- Centres of Excellence: Revolutionising dementia care research
- You are here: Newcastle University: The Pri-Dem project
- University of Exeter: The IDEAL-2 project
- Queen Mary University of London: The NIDUS project
Key outcomes
1) Identification of 20 core components of post-diagnostic support for people affected by dementia
2) Presenting a model of post-diagnostic dementia support that could be delivered by a Clinical Dementia Lead who sits within primary care
3) Indicating that future post-diagnostic support should focus on three key strands:
- Developing and strengthening care systems;
- Delivering care and support that is tailored to the needs and priorities of individuals;
- Building staff knowledge and confidence, by providing formal and informal dementia awareness raising and training
4) Providing early evidence that the PriDem model enables people with dementia to have more personalised and holistic care plans
Background
People living with dementia are usually diagnosed through secondary care specialists such as psychiatrists and neurologists. These services are often oversubscribed and face increasing demand. Ongoing support is provided by primary care such as GPs, but these services are under-resourced and often lack specialist knowledge. Quality of care can be poorly integrated across different health and social care services and varies significantly between different locations.
In response to the inadequate care received by people with dementia after diagnosis, researchers at Newcastle University developed a primary care-led approach to post-diagnostic dementia care (PriDem) in collaboration with NHS professionals, people with dementia and carers.
PriDem ultimately seeks to improve the quality of care and maintain quality of life for people with dementia and their families.
A summary of the PriDem programme for people with lived experience can be found here in this video produced by the researchers. Care professionals and commissioners may be interested in this video, and also in this report.
Who worked on this project?
Led by Professor Louise Robinson at Newcastle University in partnership with Professor Greta Rait at University College London (UCL), PriDem involved a wide variety of specialists from both the academic and clinical worlds, including practicing GPs, old age psychiatrists, health economists, and specialists in nursing and social care.
We want to address what resources are needed to provide a better quality of care, and how these can be successfully delivered.
- Professor Louise Robinson, Alzheimer's Society Centre of Excellence, Newcastle University

What did the researchers do?
The researchers first reviewed the existing literature to identify current support and gathered the views of people with dementia, their families, and healthcare professionals on the care they provided for people living with dementia.
They identified 20 core components of good post-diagnostic care relating to five key themes (see Figure 1 below). These core components are listed under five themes:
The researchers presented a model of post-diagnostic dementia support that could be delivered by a Clinical Dementia Lead (Figure 2) who sits within primary care. As a whole, PriDem indicated that future post-diagnostic support should focus on three key strands: 1) Developing and strengthening care systems; 2) Delivering care and support that is tailored to the needs and priorities of individuals; 3) Building staff knowledge and confidence, by providing formal and informal dementia awareness raising and training.
The three strands of the intervention are implemented by Clinical Dementia Leads (CDLs) working closely with staff in primary care. This kind of lead clinician model is one that has been successfully implemented for the management of other long-term conditions such as cancer and diabetes.
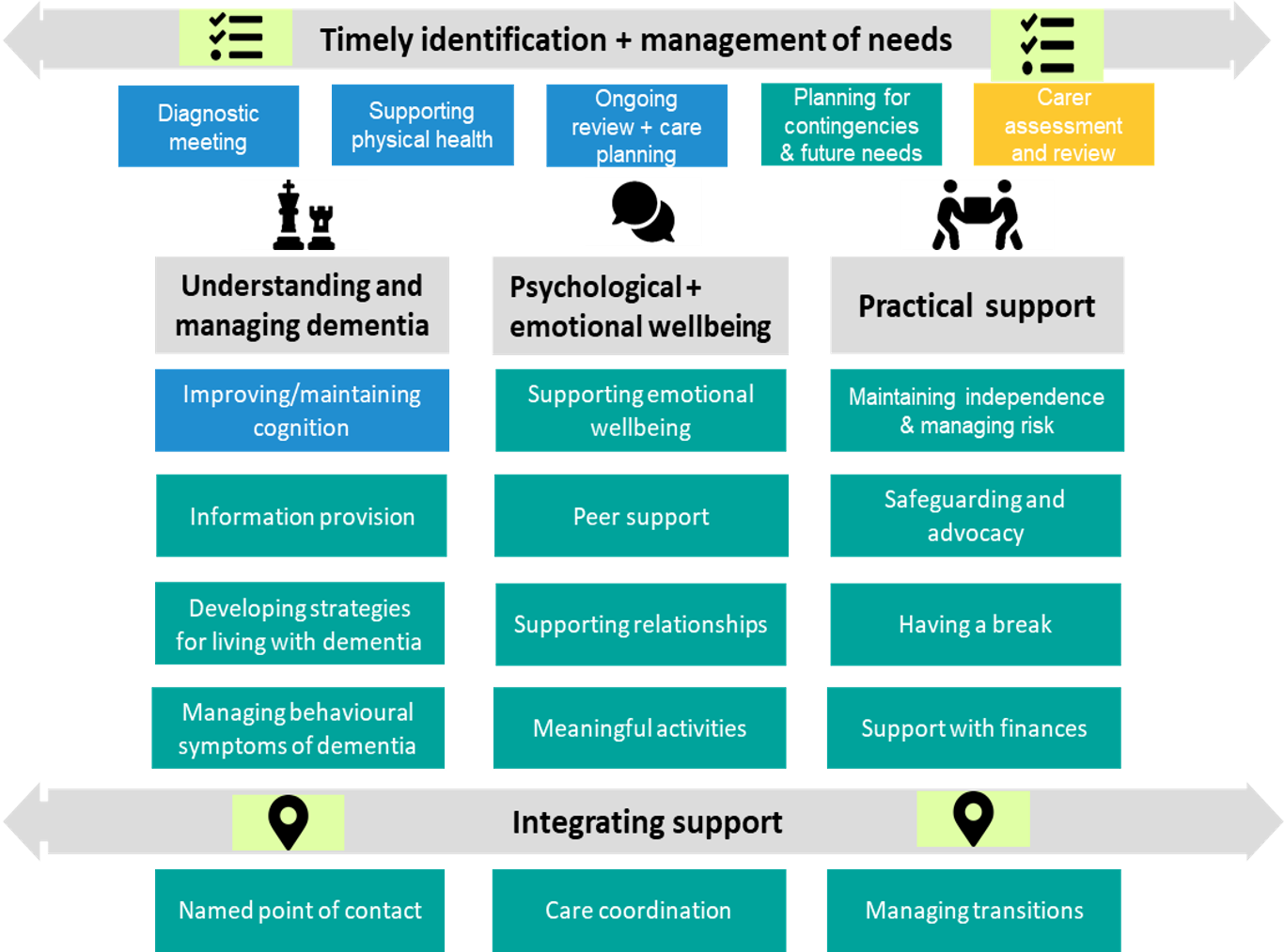
Figure 1. Key aspects of good post-diagnostic dementia care.
From PLoS One. 2021 Dec 20;16(12):e0260506. doi: 10.1371/journal.pone.0260506
They tested this model by assigning two Clinical Dementia Leads across seven GP practices in the Northeast and Southeast of England between March 2022 and June 2023. The model was accessed by 60 people living with dementia and 51 caregivers, focusing on groups who are typically underrepresented in dementia research. Patients answered questions about their quality of life when they joined the study, and then again at four and nine months.
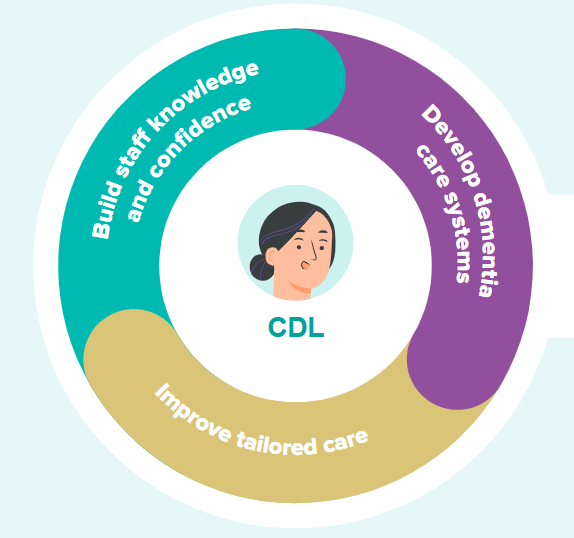
Figure 2. The role of the Clinical Dementia Lead
Key findings
Researchers collected data from professionals and people with lived experience of dementia, and used NHS criteria to define what makes a personalised care plan.
They identified seven key elements of a personalized care plan:
- The goals and outcomes of the person with dementia are recorded
- The outcomes are agreed
- The planned actions are recorded
- The review date is recorded
- The priorities of the person with dementia are considered
- Information is provided
- A copy of the care plan is provided
Before involvement in the PriDem project, just over a third of people with dementia had a personalised care plan. Participation in PriDem led to an approximate 30% increase in the number of people with personalised care plans.
The researchers also identified 12 areas of care and support that are to be included in care plans. These included:
- Services currently involved
- Information needs considered
- Social and personal history
- Home environment and activities of daily living
- Activities and interests
- The dementia diagnosis
- Cognitive, emotional, and behavioural changes
- Planning for contingencies and changes
- Progression and end-of-life care
- Safeguarding and advocacy
- Physical health
- Medication
After people with dementia participated in the PriDem project, ten out of twelve of the above areas of care were included more often in their care plans. However, for two of the areas, there was no change: medication, which was already covered in 58% of care plans, and planning for the later stages of the disease, which was included in only 5% of care plans both before and after PriDem.
Questionnaires completed by people with dementia and their caregivers showed no significant changes in their quality of life after participating in the project. This may be due to the short-term nature of the project, and collecting data at additional time points may have positive effects.
However, people living with dementia and the professionals involved in the project revealed that personalised care planning is valuable. It benefits patients and healthcare professionals, and services should be tailored to meet the needs of those using them.
For personalised care plans to be successful, GPs and other dementia care professionals need enough time and resources to focus on creating these plans. It's also important to balance flexibility in using the model without losing sight of its essential structure. How the model is put into practice might depend on the resources and services available in each local area.
What does this mean for policy and practice?
PriDem is a significant step forward in improving support for people with dementia after their diagnosis. It brings together important elements of high-quality care, with care planning being an essential component. Embedding personalised care plans across healthcare worked well for both professionals and families and led to more person-centered care that addressed important aspects of living with dementia.
The lessons from this project can be used to further develop models of post-diagnostic support that are tailored to the needs of people with dementia while ensuring continuity of care.
Details
Lead researcher: Professor Louise Robinson
Institution: Newcastle University
Themes addressed: Support after a diagnosis
Amount committed: £1,680,224 over four years
PriDem project summary
You can read our helpful 4-page booklet here to get an overview of the PriDem project.







The illness trajectory of dementia varies across and within subtypes; this difference means that tailored support is essential from diagnosis to end of life. This requires regular review to identify emerging needs and plan how to address them.
Components within this theme are:
This theme comprises components to ensure people with dementia and their carers are fully informed about their condition, what to expect, and how to live as well as possible. This includes pharmacological and non-pharmacological treatment options, many of which are evidence-based and recommended in NICE guidelines.
The components of this theme are:
In addition to providing interventions for managing psychological symptoms and supporting adjustment to a dementia diagnosis, components within this theme relate to maintaining a sense of identity and purpose through peer support groups, social and leisure activities, and supporting relationships.
The components of this theme are:
This theme covers components which focus on enabling people with dementia and carers to live independently and safely for as long as possible. While some elements of this theme focus on the needs of the person with dementia (such as support with activities of daily living or provision of assistive technology) or the carer (such as having a break), all of the components in this theme are relevant to both people with dementia and their families:
Given that multiple organisations are involved in delivering the components of post-diagnostic support described above, mechanisms are needed to ensure that services are well integrated and coordinated throughout the entire dementia journey. This theme therefore relates to integration of post-diagnostic support and comprises three components: