People living with dementia kept in hospital unnecessarily
Almost a third of people aged 65 and over who are fit to be discharged but are kept in hospital for at least three weeks longer than necessary are believed to have dementia.
New data about delayed discharge from hospital released
We have today published – for the first time – data revealing the true extent of delays to discharge from hospital for people living with dementia.
The NHS England data, analysed by HSJ Information and Alzheimer’s Society, show that around almost a third of people aged 65 and over who are fit to be discharged but are kept in hospital for at least three weeks longer than necessary are believed to have dementia. Read the full analysis.
Delayed discharge from hospital happens when someone is deemed medically fit for discharge but is unable to return home for other reasons. It reduces the numbers of beds available, creating bottlenecks that affect other parts of the NHS and exacerbates current winter pressures.
Staying in hospital unnecessarily increases a person’s risk of complications and can be especially damaging for people living with dementia, who are more likely to struggle with the unfamiliar and often distressing hospital ward environment. Read about Martin’s experience.
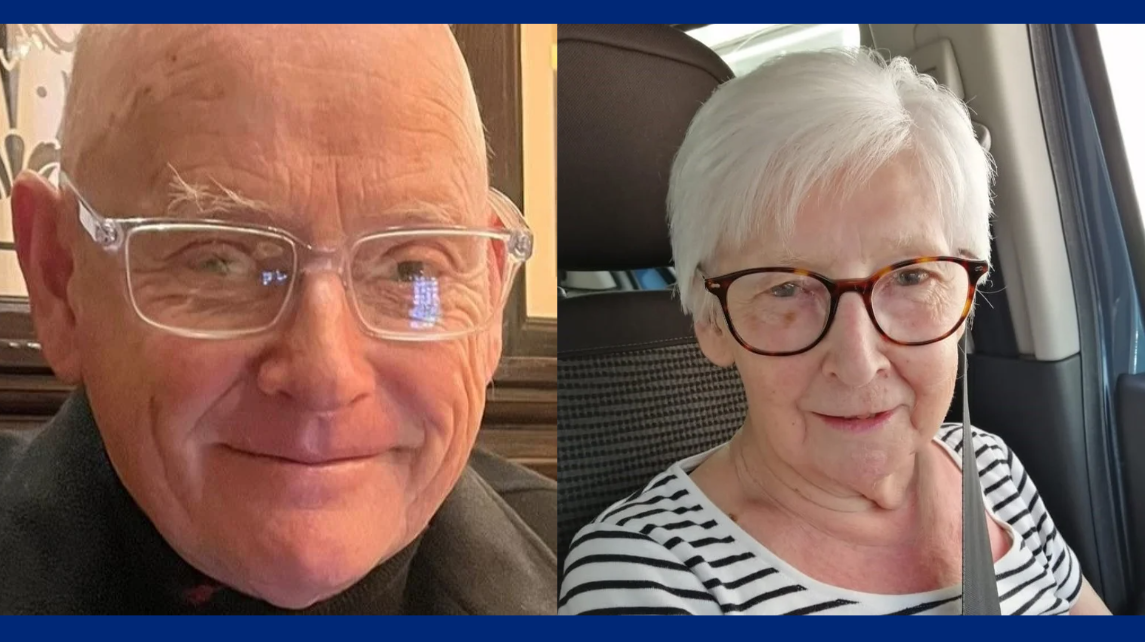
Martin and his mum, Sarah
What our Chief Executive Officer thinks
Michelle Dyson CB, Chief Executive Officer of Alzheimer’s Society said: 'Every year, the NHS faces extreme winter pressures and we see time and time again the struggle to cope with the numbers of people needing urgent care.
'It is clear from these figures that dementia is a key part of the puzzle.
People living with dementia are being left stranded in hospital, which is neither good for them nor the NHS.
'Tackling dementia care and support would make a huge difference to the NHS’s ability to cope at this time of year. Early diagnosis and access to appropriate services can help to prevent hospital admissions in the first place, while better care and support would also mean those in hospital could leave when they are well enough.
'The Government has a once-in-a-decade opportunity to fix this as it prepares its new blueprint for dementia health and social care, the Modern Service Framework. Dementia is the UK’s biggest killer and the greatest challenge facing health and social care services.
'The new plan must rise to the magnitude of the challenge, improving care to keep people healthier for longer and ultimately reduce the devastation caused by dementia.'
Response from the Chief Executive of Care England
Professor Martin Green OBE, Chief Executive of Care England, said: 'The system is not working for people with dementia and I am very grateful for the important work Alzheimer's Society is doing to bring this issue to light.
Social care should be seen as a critical partner to the NHS, receiving the funding needed to deliver the best outcomes for people living with dementia.
'This is particularly important in the context of winter pressures; the capacity in social care needs to be utilised in order to ease pressure on the NHS and deliver for patients.'
What the Chair of Alzheimer’s Society’s Clinical Advisory Group says
Adam Gordon, Professor of the Care of Older People at the Academic Centre for Healthy Ageing, Queen Mary University of London, and Chair of Alzheimer’s Society’s Clinical Advisory Group, said:
'These figures paint a stark picture of delayed discharge from hospital for people living with dementia. As a practicing clinician, I see the real trauma that these delays cause to people living with dementia and their families.
'The knock-on effect caused by unnecessary additional pressure on the NHS during its busiest winter months makes it difficult for us to give our patients the care they deserve.
That’s why we need to address the root causes of avoidable hospital admissions, by improving early and accurate diagnosis, and the quality of care and support people living with dementia receive.
'We also need more timely and expert care for people living with dementia when they need to come into hospital to ensure they can return home promptly and in the best possible health.
'The Modern Service Framework for Frailty and Dementia offers a vital opportunity to fix these foundations through a clear focus on improving dementia care pathways. We must make the most of this opportunity.'
Delayed discharge from hospital
Figures show the true extent of delays to discharge from hospital for people living with dementia.








